
1. What is geriatric medicine?

Geriatric medicine, also known as geriatrics, is a specialized field of medicine that focuses on the prevention, diagnosis, treatment, and management of health conditions that commonly affect older adults. As people age, they become more vulnerable to a variety of health problems, including chronic diseases, cognitive decline, mobility issues, and social isolation. Geriatric medicine is concerned with promoting healthy aging and maximizing the quality of life for older adults.
2. What’s the difference between a geriatrician and a medical doctor?

A geriatrician is a medical doctor who specializes in the care of older adults, whereas a medical doctor, also known as an allopathic physician, can specialize in a wide range of medical fields. Geriatricians have completed additional training in geriatric medicine beyond their general medical education, and they have a deep understanding of the unique healthcare needs of older adults.
Geriatricians typically work with a team of healthcare professionals, including nurses, social workers, physical and occupational therapists, and others, to provide comprehensive care that addresses all aspects of an older adult’s health. They are skilled in the management of multiple chronic medical conditions, as well as cognitive and functional decline, and can offer support to both patients and their families.
In contrast, medical doctors can specialize in many different areas, such as cardiology, pediatrics, or oncology. While they have a general understanding of healthcare needs across the lifespan, they may not have the same depth of knowledge and training in the specific healthcare needs of older adults that geriatricians do.
Overall, geriatricians are uniquely qualified to provide specialized care to older adults and can offer tailored medical treatments and interventions that consider the complex interactions between physical, mental, and social factors that affect their patients.
3. What are the common geriatric medicine topics?
Dementia
Dementia is a common topic in geriatric medicine, as it is a condition that affects many older adults. Dementia is a term used to describe a decline in cognitive function, such as memory loss, difficulty with language, and problems with decision-making, that is severe enough to interfere with daily activities. Alzheimer’s disease is the most common cause of dementia, but there are many other types of dementia, such as vascular dementia and Lewy body dementia.
Geriatricians play an important role in the diagnosis and management of dementia in older adults. They may work with a team of healthcare professionals, including neurologists, neuropsychologists, and social workers, to evaluate the patient and develop a treatment plan.
The treatment for dementia may involve medication to manage symptoms, as well as non-pharmacological interventions, such as cognitive rehabilitation, occupational therapy, and support for the patient and their family. Geriatricians may also help educate the patient and their family about the disease and how to manage its symptoms, and provide guidance on end-of-life care planning.
Overall, dementia is a significant health concern in the geriatric medicine context, and geriatricians play an important role in providing comprehensive care to patients with this condition.
Falls Injuries

Three out of 10 people over 70 fall annually, and 90% of broken hips in people over 70 result from falls. Therefore, geriatricians always provide a fall assessment to help seniors discover and address their fall risk factors.
Falls and fall-related injuries are a major concern in geriatric medicine, as they are a leading cause of injury and death among older adults. As people age, changes in physical and cognitive function, as well as the use of certain medications, can increase the risk of falls and fall-related injuries.
Geriatricians are trained to identify and manage risk factors for falls in older adults, and may perform a fall risk assessment as part of a comprehensive geriatric assessment. This assessment may include a review of the patient’s medical history and medication use, as well as an evaluation of the patient’s balance, mobility, and cognitive function.
Based on the results of the fall risk assessment, geriatricians may recommend interventions to reduce the risk of falls, such as exercise programs to improve strength and balance, home safety modifications to reduce fall hazards, and medication adjustments to reduce the risk of dizziness or other side effects that can increase fall risk.
Incontinence – the inability to control bodily elimination

Incontinence, or the inability to control bodily elimination, is a common condition among older adults and is often a topic of focus in geriatric medicine. Incontinence can have a significant impact on an older adult’s quality of life, leading to social isolation, depression, and a decreased ability to perform activities of daily living. Geriatricians may conduct a comprehensive evaluation to identify the type and cause of incontinence, which may include a review of the patient’s medical history, medication use, and physical exam.
Treatment options may include behavioral interventions, such as pelvic floor exercises and timed voiding, as well as medication or surgical options in some cases. Geriatricians may also provide education and support to patients and their families to help manage the physical and emotional aspects of incontinence and to promote optimal health and quality of life. Overall, incontinence is an important area of focus in geriatric medicine, and geriatricians play a critical role in identifying and managing this condition in older adults.
4. Why is geriatric care essential?

Geriatric care is essential because it is focused on meeting the unique healthcare needs of older adults. As people age, they experience changes in physical and cognitive function, and they may develop chronic health conditions that require specialized management. Geriatric care is designed to provide a comprehensive approach to care that addresses the complex health and social issues that are common among older adults.
Geriatric care can help improve the quality of life for older adults by providing individualized care that considers the patient’s overall health and wellbeing. This may include managing chronic conditions, preventing and managing falls and other injuries, addressing mental health concerns, and promoting healthy lifestyle behaviors. Geriatric care can also provide support for caregivers and family members, who may be dealing with the challenges of caring for an aging loved one.
In addition, geriatric care can help reduce healthcare costs by improving health outcomes and preventing unnecessary hospitalizations and emergency department visits. This is particularly important given the growing population of older adults, which is expected to increase in the coming years.
5. Is geriatrician in demand in Malaysia?
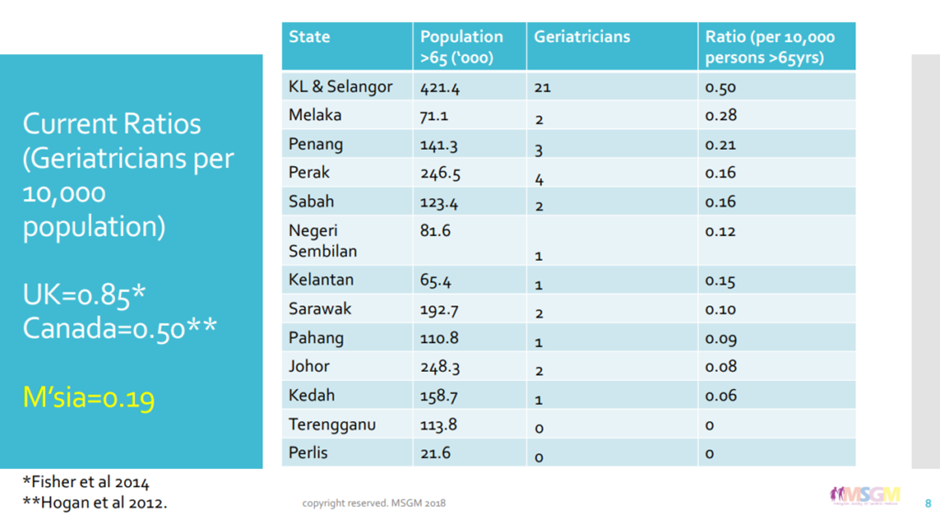
Certainly. Malaysia, like many other countries around the world, is facing a growing population of older adults, which makes geriatric care an urgent need. However, according to the Malaysian Society of Geriatric Medicine (MSGM), the country has a shortage of senior specialists, with a geriatrician ratio of only 0.19 per 10,000 population, which is far below the levels seen in developed countries such as the United Kingdom (0.85) and Canada (0.5). This shortage of geriatric specialists can make it difficult for older adults in Malaysia to receive the specialized care they need to maintain their health, independence, and quality of life. It is crucial for the government and healthcare industry in Malaysia to invest in geriatric care and to train and recruit more geriatric specialists to ensure that the country’s aging population receives the best possible care.
6. What age are you considered a geriatric?
The minimum age varies across different countries. In Malaysia, a person is considered geriatric once they reach the age of 60.
7. Is there any special case?
Although most geriatricians treat the elderly, there are also exceptional cases when:
a. They have complex illnesses
When a patient is diagnosed with multiple diseases simultaneously, for instance, a patient diagnosed with type 2 diabetes may eventually develop kidney disease or diabetic retinopathy at an early age
b. They are taking too many medications
Plenty of medications will follow if the patient develops different types of diseases. Geriatricians ensure that the medicines do not cause drug-drug interactions, in which two drugs react with each other and stimulate a series of adverse side effects. They weigh every drawback of treatments against your quality of life and decide the best solution for you.
8. Do geriatricians treat mental issues?

Yes. Geriatricians work on more than just the physical health of patients. They also promote healthy social relationships, boost cognitive abilities, and help patients become independent. To a certain extent, they assist in legalities, such as drafting living wills or choosing a primary caregiver.
9. How to choose the right senior doctor?

a. Get a doctor who is willing to share information
Getting a doctor willing to share information with you and your caregivers is essential. In certain situations, we can assume that a doctor who willingly shares information is a doctor who cares about their patient’s well-being. Find the one you can work with and who is likely to provide outstanding care that others won’t.
b. Research the geriatrician’s credentials
Board certification is one of the most important factors to consider when you are choosing a geriatrician. It tells you whether the geriatrician has the necessary training, skills and experience to provide healthcare in geriatric medicine. Also, confirm that the geriatrician has no history of malpractice claims or disciplinary actions.
10. How to find a geriatrician in Malaysia?
You can find your ideal geriatrician in Malaysia through DoctorOnCall. It allows you to consult their geriatricians through chat, video or audio calls from RM19.99. At the same time, you can receive a prescription and have the medicine delivered to your doorstep.
References
https://codeblue.galencentre.org/2021/11/24/malaysias-ageing-population-finds-shortage-of-doctors/
https://www.docdoc.com/medical-information/specialties/geriatrics
https://blog.ioaging.org/aging/secret-choosing-right-geriatric-doctor/
https://www.healthgrades.com/right-care/aging-well/8-tips-for-choosing-a-geriatrician
https://www.webmd.com/a-to-z-guides/what-is-geriatric-doctor
A Pillar of Strength in Golden Years: 10 Paths on How Regular Screenings Uphold Your Health
In the evocative voyage of life, the golden years emerge as a time to relish the fruits of decades of labor, to bask in the
Unlock the Secret to Sweet Dreams: 10 Ways of Enhancing Sleep Quality as You Age
Share on facebook Facebook Share on twitter Twitter Share on linkedin LinkedIn Share on pinterest Pinterest Share on telegram Telegram Share on whatsapp WhatsApp Share
Building Bridges, Not Walls: 10 Methods of Mastering the Art of Cultivating Social Connections in the Golden Years
Share on facebook Facebook Share on twitter Twitter Share on linkedin LinkedIn Share on telegram Telegram Share on whatsapp WhatsApp Share on email Email Share
Navigating the Golden Years: 10 Ways to Achieve Emotional Wellness and Conquering Loneliness
Share on facebook Facebook Share on twitter Twitter Share on linkedin LinkedIn Share on pinterest Pinterest Share on telegram Telegram Share on whatsapp WhatsApp Share
Stay Brainy in Your Golden Years: 10 Fun Activities to Keep Your Mind Sharp and Engaged!
Hello, brain buffs! Aging might be inevitable, but letting our minds turn to mush? No way, José! Time to boot up those brain cells and
10 Effective Exercise Routines for Older Adults: Low-Impact Fitness Options
Of course, maintaining physical health is crucial at any age, but especially so as we grow older. Here are ten gentle, effective, and friendly exercise